Coronary Artery Calcification and Complications in Patients With COVID-19
JF. Gautier has recently contributed to a cross-sectional study at Lariboisière Hospital, in relation to coronary artery calcification and complications in patients with COVID-19.
In the COVID-19 pandemic, early risk stratification of severe forms is essential. Patients with COVID-19 and cardiovascular risk factors have higher morbidity and mortality. In patients at high cardiovascular risk, coronary artery calcification (CAC) is associated with a higher incidence of nonfatal and fatal outcomes. Chest CT has become a key tool for the diagnosis of COVID-19, but CAC detection is not carried out routinely.
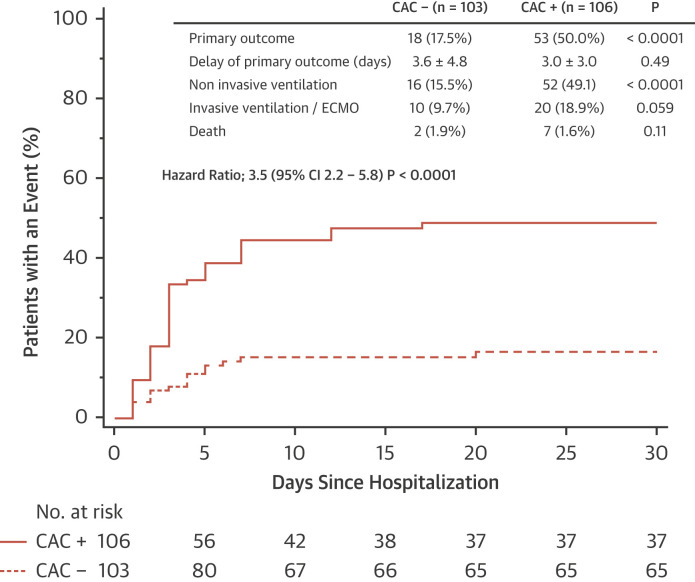
From March 15, 2020 to May 3, 2020, authors performed a cross-sectional study including consecutive patients hospitalized with COVID-19, 40 to 80 years of age, who underwent non-contrast chest computed tomography on the day of admission. The presence or absence of CAC (CAC+ and CAC−, respectively) was analyzed. Agatston score was also measured. Analysis was performed by 2 certified operators blinded to clinical history (1 radiologist and 1 cardiologist). The primary outcome was the first occurrence of mechanical noninvasive or invasive ventilation, extracorporeal membrane oxygenation, or death within 30 days following hospital admission. Because CAC is highly correlated with age, the primary outcome was segmented by median age group.
CAC was detected in 106 of 209 patients (50.7%). The primary outcome occurred in 50.0% of CAC+ patients compared with 17.5% of CAC− patients (p < 0.0001). CAC was significantly associated with the primary outcome. Among patients <62 years of age (n = 104), CAC was detected in 32%, and the primary outcome occurred in 55% of CAC+ patients compared with 20% of CAC− patients. Among patients ≥62 years of age (n = 105), CAC was detected in 69%, and the primary outcome occurred in 48% of CAC+ patients compared with 13% of CAC− patients. In a multivariate analysis with a Cox proportional hazards model including age, sex, hypertension, smoking, and diabetes, CAC was independently associated with the primary outcome.
The median Agatston score was 8; 28.7% of patients had Agatston scores >100, and 2.9% had scores >400. The crude HR for the primary outcome for Agatston score (per quartile) was 1.6 (95% CI: 1.3 to 2.0; p < 0.0001), and using the same Cox proportional hazards model, the HR for Agatston score was 1.8 (95% CI: 1.5 to 2.3; p < 0.0001). In CAC+ patients, mean calcification density was 457 ± 176 HU in patients without events, compared with 387 ± 153 HU in patients with events (p = 0.03)
This study shows that the presence and extent of CAC are associated with a worse prognosis in hospitalized patients with COVID-19. The severity of immune response, endothelial dysfunction, and myocardial stress due to COVID-19 could be exacerbated in patients with subclinical coronary atherosclerosis.
To read the full paper, head to the following link:
https://www.sciencedirect.com/science/article/pii/S1936878X2030601X